! BLACK FRIDAY - OFFER EXTENDED !
🖤10% OFF BIO-STIMULATORS (including courses!) click here 🖤 10% OFF POLYNUCLEOTIDES (including courses!) click here
To take advantage of these BLACK FRIDAY DISCOUNTS - payment needs to be made by 05/12/2025 and treatment must be taken or started by 06/03/2026.

Cryotherapy Lesion Removal
Unfortunately, the NHS no longer fund the removal of cosmetic lesions, but we can help. Cryotherapy freezes and destroys a wide variety of skin blemishes and lesions with effective, permanent results.
Quick and easy procedure - Low risk and accurate.
SUITABLE
✓ Solar lentigines: Age and sunspots, liver spots, freckles
✓ Viral Lesions: Warts & Verrucas
✓ Cherry angioma (blood spot)
✓ Sebaceous Hyperplasia (enlarged sebaceous gland)
SUITABLE IF PRE-CHECKED
✓ Seborrheic keratosis (brown warts, non-contagious) *
✓ Benign Moles *
✓ Skintags *
✓ Angiofibroma (fibrous papules) *
✓ Granuloma (inflamed nodules) *
✓ Dermatofibroma (benign fibrous skin growths) *
✓ Molluscum contagiosum (water warts) *
✓ Porokeratosis (dermatosis) *
✓ Actinic keratosis (pre-cancerous skin lesions) *
NOT SUITABLE
X Condyloma acuminate (genital warts)
X Actinic keratosis (pre-cancerous skin lesions)
X Malasma
X Under the age of 14
* You need written confirmation from a licensed medical practitioner, such as a dermatologist or GP that any skin cell growths (skin tags, moles, or other growths) are non-malignant prior to removal. GP's sometimes charge a small fee for this. If you are in a hurry, we have a registered dermatologist service for £60, reports come back within 48 hours, click here for more information.
Very small skin tags, tags with stalks, blood spots and milia can also be treated with diathermy Laser treatments are also available for pigmentation click here.
What to do before you book?
1) Read the FAQ's below to check you are suitable and happy to go ahead
2) Get written confirmation the lesion is non-malignant before you book *
3) Its useful to send us a photo of the lesion (in good natural lighting).
Frequently asked questions
The process is called cryo-necrosis, tissue destruction by freezing. Tissue destruction occurs when cells are low in temperature and at least -80F and ice crystals will form. The ice crystals break the cell membrane, destroy cells organelles and protein matrixes. Water then rushes into the surrounding area causing blistering and disruption of the local blood supply. The innovation of CryoPen® is the direct application of nitrous oxide under high pressure (55 bar).
You will have a consultation to check you are suitable and any questions are answered, and then a pre-treatment photo will be taken. The area will be cleaned and the lesion will be treated. It can take around 1 to 15 minutes to remove a lesion. For example, larger tissue growths such as skin tags and moles take more time. A protective soothing product is be applied and aftercare advice is given.
Cryotherapy is quicker than other treatments and patients can be in and out in seconds. It requires no anaesthesia and has minimal scarring. There are no limitations on activity except to protect the area from damage or abrasion, they can work, bathe, swim, immediately after the treatment. There are not cuts, bleeding, sutures and risk of infection.
Care should be taken when treating areas with very thin skin and areas where the colour is cosmetically important such as face, ears, scrotum and lateral surface of fingers.
Viral lesions are the hardest to treat because you are treating the lesion as well as the virus. In the days leading up to the appointment, it is recommended to do a pre-treatment to the wart or verruca to prepare it for the best possible treatment. The treatment works best when the skin covering these lesions is soft and slightly opened.
Follow the steps to allow the treatment to work effectively.
• Soak the lesion in a bowl of warm, soapy water for 20 minutes.
• With a pumice stone or emery board (nail file), gently scrub the lesion until the skin becomes rough. (Remember to throw the item away after use).
• Please do not scrub so hard that you make the area sore. Discontinue these steps if bleeding occurs.
You are not trying to open a wound or cause discomfort. However, the more deeply the jet of nitrous oxide can penetrate, the better the chances of removal are.
CryoPen® uses disposable cartridges of liquefied N2O to deliver quick, effective cryotherapy treatments to benign skin lesions. Temperature of nitrous oxide is -89°C; it destroys tissue by freezing the intercellular fluid and forming ice shards and crystals that rupture the cell membrane, destroying the cell.
•Versatile treatment options, treats lesions from 1mm to 10mm in size • Fast treatments, treats a 2mm lesion in 10 seconds • Penetrates deeply into lesion (up to 5mm deep) • Safely treats lesions on face and close to eyes • Pinpoint accuracy, treats just the lesion and not healthy surrounding tissue • Can treat longer, with fewer repeat visits • Doesn’t touch skin (no messy buds, cones or apertures) • Enhanced accuracy.
Yes, the CryoPen® is FDA and CE approved. We use the best equipment available... The market-leading CryoPen devices are created and manufactured in Belgium and have been producing cryosurgery medical instruments for the last 24 years.
A typical freeze on viral infections may last from 5 to 10 seconds for a small flat wart and up to 45 seconds for a full thickness plantar wart. For general purposes, most lesions take about 2 to 30 seconds.
Avoid ANTIHISTAMINES (unless medically prescribed) 48 hours before and 24 hours after treatment (histamine is required in the body, as it is part of the inflammatory response during the skin healing process).
Bring your GP/dermatology letter with you which states the skin growth/lesion is non-cancerous or use our Mole Screening service.
Soften and file down warts and verruccas as much as you can without making the skin bleed the week before.
No anaesthesia is needed as the extreme cold causes anaesthesia which allows the treatment to be tolerable.
Melanocytes are the most sensitive to cold injury. Therefore, they are the most easily damaged with cryotherapy. Dark-skinned patients need to consider the risk of permanent loss of pigment.
Yes, for age 12+ with parental consent and presence required.
At a penetration rate of 1mm per 5 seconds, the ice will reach the caudal extent of the lesion after a given amount of time related to the depth of the lesion. It can feel like a ballpoint pen being pushed into the skin From that moment, the patient will experience a pain sensation. There might be a little residual stinging for a few minutes after treatment.
Patients may experience inflammation/swelling, crusting/scabbing, blistering, erythema, heat/warmth around the treated area, or darkening of the lesion for a period of usually 7-14 days post-treatment and potentially up to 4 weeks depending on the area being treated, intensity of treatment and skin health prior to treatment.
Lesions on the body generally have a longer healing time as those on the face.
After the treatment, the treated area may look reddish, itch, and it is not uncommon for a blister to form withing a few hours. The blister can appear either clear or with a reddish or purplish shade. It is common to experience mild discomfort or pain in the treated area for the next few days following treatment.
Blister
Within the next couple of days, it is possible for a blister to develop as a result of cryosurgery. It is important not to intentionally open the blister, as it serves a purpose in allowing the separation and removal of the skin lesion from the surrounding healthy skin. The blister may contain clear or bloody fluid. It is normal for the treated area to be sensitive and cause discomfort for a few days. If needed, the client may need to revisit the clinic for drainage of the blister – again should we delete this, we would have people getting clients back to pop blisters, should be referring to their GP if this is required. In the event that the blister pops, it is advised to clean the site twice a day using a saline solution or tap water, or use an alcohol-free wipe, and gently dab or wipe the skin with it. Apply a smear of antiseptic cream. It may also be covered with a dressing/plaster. In general, it doesn’t require any special scare during the healing process. Gently wash the area once or twice a day, keeping it clean is important. The use of a bandage or dressing may only be necessary if the area is prone to rubbing against clothing or if there is a risk of easy injury.
Swelling
Swelling is a typical occurrence after cryosurgery, particularly around the eyes, forehead, and nose. If swelling does occur, there is no need for alarm. You can apply cool tap water-soaked towels to the affected area if required. Typically, the swelling will reduce over a period of 3-10 days. However, if the swollen area is both tender and swollen, it may indicate infection and should be reassessed by a healthcare professional.
Eschar (scab)
Eschar, also referred to as the “scab”, forms following cryosurgery. It is advisable to leave the large eschar undisturbed for as long as possible. It will naturally peel away on its own within 1-3 weeks, depending on the treated area once the underlying tissue has sufficiently healed. It is important not to pick at the scab, as it could disrupt the healing process and potentially lead to scarring. This natural protective barrier serves aiding in the healing process by maintaining a moist environment and facilitating the building of growth factors and formation of new granulation tissue. The liquid drainage from the eschar contains essential growth factors that contribute to advancing the healing process and promoting overall healing. In some cases, bleeding may occur after the procedure. If client experiences bleeding, advise them to gently apply firm and steady pressure using a dry cloth for 20 minutes or until the bleeding has stopped.
Infection
In the healing process, it is normal to observe a certain degree of redness and drainage as new blood vessels form. However, if client suspects that the site may be infected, ask them to reach out to you for assistance. Recognising the signs of infection is important in order to seek appropriate medical attention. Some indicators of infection include continuous swelling, ongoing pain, excessive redness, significant warmth around the wound, and unusual drainage. Additionally, infected wounds tend to be overly tender to touch. For these symptoms, you should promptly notify a healthcare professional for evaluation and necessary treatment.
If your lesion does not scab, it does not mean it was not successful, as all lesions respond differently and some only swell, before another session is required aprox 4 weeks later.
In some cases, at 4 weeks the area may still be settling, and it can be pink or slightly uneven for up to 8–12 weeks and in rare cases longer.
We cannot guarantee the success of treatment or the outcome that you may have.
Typically, it leaves the least amount of scarring of any form of lesion removal because it causes the least damage to the connective tissues. Although rare, scarring is a possibility.
Hypopigmented lesions will be noticeable until they darken with the new tanning.
In some cases, at 4 weeks the area may still be settling, and it can be pink or slightly uneven for up to 8–12 weeks and in rare cases longer.
Post-inflammatory hyperpigmentation (PIH) can happen after Cryotherapy, and it often fades over 8–12 weeks. Sometimes takes 3–6 months or in rare cases longer.
We cannot guarantee the success of treatment or the outcome that you may have.
It is dificult to say how many sessios you may need as there are varying factors invloved.
Often, 1-2 sessions will be enough.
Larger lesions, difficult, or some raised moles may need 2-3 sessions.
Some deeper lesions may take several aggressive treatments; in particular, warts and verrucas often need multiple sessions.
For warts and verrucas, it is strongly recommended that you follow the preparation we advise before your appointment to prevent you from needing more treatments than necessary.
We can never guarantee the outcome of cryotherapy treatment but generally get very good results with the majority of lesions.
For most lesions, cryotherapy is a permanent removal. Some lesions are harder to remove than others.
Both hypopigmentation and hyperpigmentation may occur after cryotherapy. Both generally last a few months, but can be longer-lasting. Permanent colour loss can occur in dark-skinned patients.
Occasionally, a blister might form and persist for up to 5 days. After, it scabs over the lesions. Healing depends on how deep the wound is. Typically, healing occurs from 2-6 weeks, depending on the length of freeze and location.
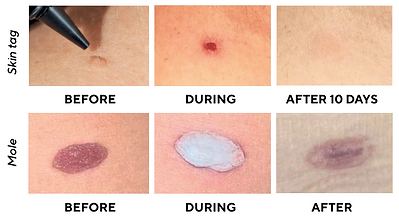
You can see images of the healing process on the main page.
Once the scab forms, your body’s immune system will start to protect the wound from infection.
During the initial stage of wound healing, the following changes occur: The wound becomes slightly swollen, red or pink, and tender. Clear fluid may be observed oozing from the wound. This fluid aids in cleansing the area. Blood vessels in the vicinity of the wound dilate, allowing blood to deliver oxygen and nutrients vital for the healing process. White blood cells come into action, combating potential infections caused by germs and initiating the repair of the wound. This stage takes about 2-5 days.
Tissue growth and rebuilding happens next. During the next 3 weeks, the body starts repairing broken blood vessels and new tissue develops. Red blood cells contribute to the creation of collagen, strong white fibres that serve as the foundation for new tissue formation The wound gradually fills in with newly-formed tissue known as granulation tissue. New skin begins to form over this tissue. As the healing process progresses, the wound edges contract inward, resulting in a reduction in size.
As the healing process advances, a scar develops, strengthening the wound: During this stage, you may experience itching on the healing area. Following the detachment of the scab, the area might appear stretched, red, and shiny. The scar that forms will be smaller than the original wound. The formed scar will be smaller in size compared the initial wound. It will be less strong and less flexible than the surrounding skin. Over time, the scar will gradually fade and may even disappear entirely. This fading process can extend up to two years. It’s important to note that some scars may never fully fade away. Scars emerge because the newly formed tissue differs from the original tissue. Superficial injuries that only affect the top layer of the skin generally do not result in scarring. However, deeper wounds are more likely to leave a scar behind.
What else can effect healing:
Generally, older adults tend to heal at a slower pace compared to younger individuals. Excessive alcohol consumption can impede the healing process, increase the risk of infection, and contribute to complications following surgical procedures.
Blood thinners If the blood is thin, the healing could be compromised. This makes the treatment healing uncertain.
Specific medication Medicines such as corticosteroids, non-steroidal anti-inflammatory medicine can slow healing.
Conditions such as arteriosclerosis (clogged arteries) or issues like varicose veins can results in inadequate blood circulation, hindering the healing process.
Underlying health concerns may affect healing time.
There are no limitations on activity except to protect the area from damage or abrasion. Swimming and showering are not a problem.
If the blister pops, the use of an antibiotic cleaning solution and ointment is recommended. Covering the area with a bandage also promotes healing.
Follow-up should be scheduled in 2-4 week intervals to observe results, and for further sessions if required.
CryoPen® Therapy is a relatively low-risk treatment and side effects and complications are usually minimal. Some side effects may occur. These include:
Pigment changes -both hypo pigmentation (lightening of the skin) and hyper pigmentation (darkening of the skin). Both generally last a few months, but can be longer lasting.
Nerve damage - though rare, damage to nerves is possible, particularly in areas where they lie closer to the surface of the skin, such as the fingers, the wrist, and the area behind the ear. Reports suggest this will disappear within several months.
Shards of frozen humidity - the high pressure jet may cause minor shards of frozen humidity in the air blown away in a circle of approximately 30cm. They thaw the moment they touch healthy skin.
Lesions on sites with coarse terminal hair - hair follicles are easily damaged by cryosurgery and permanent alopecia is not uncommon.
Blisters - patients may experience blistering for a period of 7-14 days post-treatment and potentially up to 2-4 weeks depending on the area being treated, the intensity of the treatment, and skin health prior. Lesions on the body generally have a longer healing time compared to those on the face.
Some people can have delayed healing, particularly if they have underlying health concerns.
Cryotherapy is unlikely to leave a scar, but in rare cases, a scar can form, particularly with deeper lesions. The resulting scar is often a pale or white mark, sometimes slightly depressed or, very rarely, raised (hypertrophic or keloid), and is more likely to occur with deeper freeze treatments
You will be given full written aftercare on the day
Following treatment, residual stinging, redness & slight swelling is normal. It is perfectly normal to experience these side effects, which can last for a few hours.
The area needs to be kept as dry as possible while healing. For the first 3 days, it is recommended to be careful whilst showering and to not wash the area, avoid swimming, saunas, steam rooms, sunbeds and excessive exercise causing sweating. Once scabbed , you can gently go back to your normal activities.
Use a plaster to protect high bacterial areas during the day. If the area treated is in high-bacterial areas (like the underarms or groin), your practitioner may advise wearing a plaster during the day, and to wash the area in the evening and removing the plaster at night to allow the skin to breathe.
It is normal for the lesion to turn darker or form a scab/crust. In the case of all lesions, over the next few days the area will turn darker and develop a crust on the surface. DO NOT pick this off. When it naturally falls away, you will see new skin which is a shiny pink/brown colour. This is not scarring. It will re-pigment over the following weeks and could take several months. There may be a slight difference in colour permanently.
Permanent alopecia/hair loss can occur in a treated area which was previously covered with hair.
If the area treated does not heal after 6 weeks, please contact your treatment provider.
Avoid picking at the treated area. Do not pick at the treated area at any time after treatment, otherwise the area will take longer to heal. If a scab is comes off accidentally, it will also take longer to heal, but you shoud still have the same outcome of a successful treatment.
If the scab comes off too early, check if the skin isn’t open. If it is open, this is an open wound and must be cared for to prevent infection. Put a plaster over the area to protect it and if the area becomes inflamed and produces pus, then it is infected. Use an antispetic lotion and see your GP.
Wait until the scab has healed and comes off naturally before booking another session. If the small crust has not fallen off after four weeks, please wait until it has done so before booking another session. Skin can sometimes take several weeks and even months to regenerate.
Do not use or apply any products unless advised or prescribed by your treatment provider. We do not recommend covering the area with a dressing or plaster unless we have advised you to do so. This applies to using any anti-septic creams unless there is the suspicion of an infection.
If the area being treated is tanned, please note that healed skin will be lighter. Any depigmented areas post-procedure will eventually re-pigment as it matures.
Protect the treated area and your skin with SPF. Once the scab has fallen off, please use a sunblock with SPF50 on any pigmentation removal until it has re-pigmented.
No, you need to obtain written confirmation from your GP or other licensed medical practitioners, ideally a dermatologist, that any skin cell growths (for example skin tags, moles, or other forms of growth) are non-cancerous prior to making your appointment.
Many clinics charge £100 as a consultation fee for them to check lesions are non-cancerous and then charge for the treatment on top of this fee.
GP letters can range from £0-£30.
If you are unable to wait for a GP appointment, we have a registered dermatology service 'Map My Mole'. We take magnified photos of the lesion, along with history and information and send it to the dermatologist for review, diagnosis and approval for removal. This service cost £60 per lseion (£30 for any additional lesions) and results are usually back within 48 hours.
The following are contraindications therefore treatment not suitable:
- Pregnancy or breastfeeding
- Cardiac Disease
- Chemotherapy or Radiotherapy treatment
- Raynaud disease
- Impaired wound healing e.g. blood thinners, will require a GP note of approval (blood thinners can increase sensitivity to cold and the skin can become thinner. The healing is compromised; this makes the treatment healing uncertain).
- Diabetes unstable, or type 1 diabetes will require a GP note of approval.
- Pre-malignant/malignant lesions or any skin cancer elsewhere
- Impaired sensation
- Impaired circulation
- Hypersensitivty to cold
- Open wound
- Recent scar tissue
- Prone to Keloid scarring
Antihistames - Please avoid taking them 2-3 days prior to your treatment unless medically prescribed. If it is taken for allergy reasons, seek professional medical advice before.
Redness, increased pain, yellow/green pus, or excessive clear fluid around the injury. These are signs of infection.
Black edges around the injury.
Bleeding at the injury site that will not stop after 10 minutes of direct pressure.
Fever for more than 4 hours.
Pain at the wound that will not go away, even after taking pain medicine.
If more than 1 treatment is required:
4 weekly for general lesions
2 weekly for viral lesions
It depends on the lesion and your body. Some lesions are completly removed and others are reduced and/or flattened.
There are many different types of moles including: Common Moles, Junctional Melanocytic Naevi, Dermal Melanocytic Naevi, Dysplastic Naevi, Halo Naevi, and Congenital Naevi.
Moles vary hugely and GP approval is required for all moles.
The characteristics of a normal mole will often be: SYMMETRY - Symmetrical, round or oval
BORDER - Well defined
COLOUR - Flesh coloured, light brown or dark brown
DIAMETER - Usually less than ½ cm
EVOLUTION - Stay fairly static with little change throughout the client’s life
LOCATION - Most commonly found on sun-exposed areas
UNIFORMITY - Most moles look similar
Some things to look out for:
ASYMMETRY – the two halves of the area differ in their shape. BORDER – the edges of the area may be irregular or blurred and sometimes show notches. COLOUR – this may be uneven. Different shades of black, brown and pink may be seen. DIAMETER - most melanomas are at least 6 mm in diameter.
Despite removing many lessons we are not dermatologists. You need written confirmation from a licensed medical practitioner, such as a dermatologist or GP that any skin growths are non-malignant prior to removal.
You cannot have treatment without this confirmation. We keep this letter securely on your file.
Applicable to the following:
Seborrheic keratosis (brown warts, non-contagious) *
Benign Moles *
Skintags *
Angiofibroma (fibrous papules) *
Granuloma (inflamed nodules) *
Dermatofibroma (benign fibrous skin growths) *
Molluscum contagiosum (water warts) *
Porokeratosis (dermatosis) *
Actinic keratosis (pre-cancerous skin lesions) *
At Westfield Clinic we take this seriously, and have the following in place:
🏥Practice License with Local Council
👩🏫ICO member (Information Commissioner's Office) Regulates Data Protection and Information Rights
🏥GDPR Regulations adhered to
📝Risk Assessment updated regularly
📄Covid Risk Assessment
💊MHRA (Medical Healthcare Regulatory Agency) laser equipment
🏥Local Rules from LPA (Laser Protection Advisor) for safe laser use
🏥LPA Site Audit Report
👩🏫LPS (Laser Protection Supervisor) appointed
☑️ CE Certified Equipment
🔌PAT Testing all electrical equipment
👩🏽🔧Laser equipment routine servicing and calibration
🕶️Certified Eye protection for each laser wavelength
🎓Cok (Core of Knowledge) Laser updated 3 yearly
🎓CPD and Ofqual Qualifications regularly updated
🏥Member of BMLA (British Medical Laser Association)
🔥Co2 and Foam Fire Extinguisher regularly serviced
⛑️Laser & Fire Safety Signage
💉Sharps and Hazardous Waste collection

















Gallery





















What does it cost?






















happy and I high recommend to anyone.




Clinic for a long time. Liana is lovely and very knowIegable about all her treatments. I always feel relaxed and confident that all the correct guidelines are being followed. I would recommend Liana to my family and friends.






I felt very comfortable during the consultation.

Testimonials



Liana has a friendly manner which puts you at ease. She is totally professional, keeps uptodate with training and shares her knowledge by talking through and explaining the procedures. I have every confidence in her and always leave the salon feeling relaxed and pampered.















The Healing Process